Understanding the Molecular Mechanisms Underlying Alzheimer’s Disease

BioE Chair and Professor Lee Makowski, in collaboration with Massachusetts General Hospital, received an NIH $2.1M award for “Fibrillar Polymorphs in Human Brain Tissue.” Working with neuropathologists from MGH, his research group will be using x-ray scanning microscopy to observe changes in the molecular structure of amyloid plaques and neurofibrillary tangles during disease with the goal of better understanding the molecular mechanisms underlying the disease. Identification of the molecular interactions driving disease should provide clues to aid in the design of therapeutics to slow or halt disease progression.
Alzheimer’s disease is a neurodegenerative disorder in which deposits of abnormal fibrillar aggregates accompany the spread of neuronal damage during disease progression. A central hypothesis of this project is that the role of these fibrillar aggregates may be clarified by observing them in the context of diseased tissue. To do this, a multidisciplinary team will use methods that generate detailed information on fibril structure and organization while preserving information on their locations across multiple length scales.
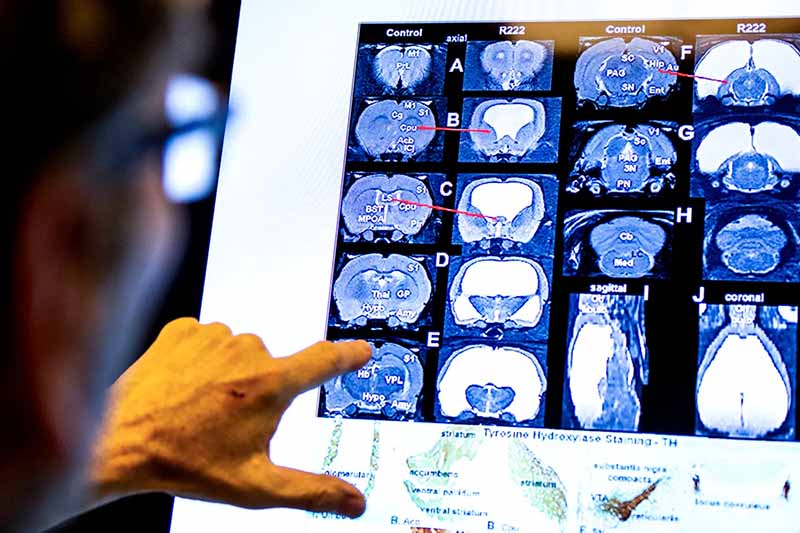
Photo by Ruby Wallau/Northeastern University
View the full article “New Research Could be Key in Unlocking Better Treatment for Alzheimers” by Northeastern Global News
Abstract Source: NIH